(Managing Dawn Phenomenon with Basal Insulin is excerpted from Think Like A Pancreas: A Practical Guide to Managing Diabetes With Insulin by Gary Scheiner MS, CDE, DaCapo Press, 2011)
The liver is a fascinating organ. It does about a hundred different things. One of its main functions is to store glucose (in a dense, compact form called “glycogen”) and secrete it steadily into the bloodstream in order to provide our body’s vital organs and tissues with a constant source of fuel. This is what keeps your heart beating, brain thinking, lungs breathing and digestive system, uh, digesting, pretty much all the time.
In order to transfer the liver’s steady supply of glucose into the body’s cells, the pancreas normally secretes a small amount of insulin into the bloodstream every couple of minutes. This is called basal insulin. Not only does basal insulin ensure a steady energy source for the body’s cells, it also keeps the liver from dumping out too much glucose all at one. Too little basal insulin, or a complete lack of insulin, would result in a sharp rise in blood sugar levels.
So, you might say that basal insulin and the liver are in “equilibrium” with each other. The basal insulin should match the liver’s secretion of glucose throughout the day and night. In the absence of food, exercise and rapid-acting/mealtime insulin, the basal insulin should hold the blood sugar level nice & steady.
Each person’s basal insulin requirement is unique. Typically, basal insulin needs are highest during the night and early morning, and lowest in the middle of the day. This is due to the production of blood sugar–raising hormones during the night, and enhanced sensitivity to insulin that comes with daytime physical activity. Two hormones in particular – cortisol and growth hormone – cause the liver’s natural ebb and flow in glucose secretion.
During a person’s growth years (prior to age 21), basal insulin needs tend to be relatively high throughout the night, drop through the morning hours, and gradually increase from noon to midnight. Most adults (age 21+) exhibit an abrupt increase in basal insulin requirements during the early morning hours, followed by a drop-off until noontime, a low/flat level in the afternoon, and a gradual increase in the evening. This peak in basal insulin during the early morning hours is commonly referred to as a dawn phenomenon.
Basal insulin can be supplied in a variety of ways. Intermediate-acting insulin (NPH) taken once daily will usually provide background insulin around the clock, albeit at much higher levels 4 to 8 hours after injection and at much lower levels at 16 to 24 hours. Long-acting basal insulins (glargine and detemir) offer relatively peakless insulin levels for approximately 24 hours. Insulin pumps deliver rapid-acting insulin in small pulses throughout the day and night. With a pump, the basal insulin level can be adjusted and fine-tuned to match the body’s ebb and flow in basal insulin needs. It is also possible to combine various forms of long-acting insulin to simulate the body’s normal basal insulin secretion.
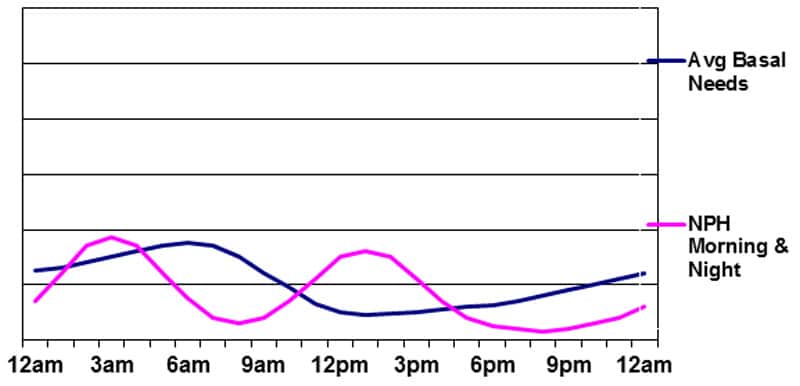
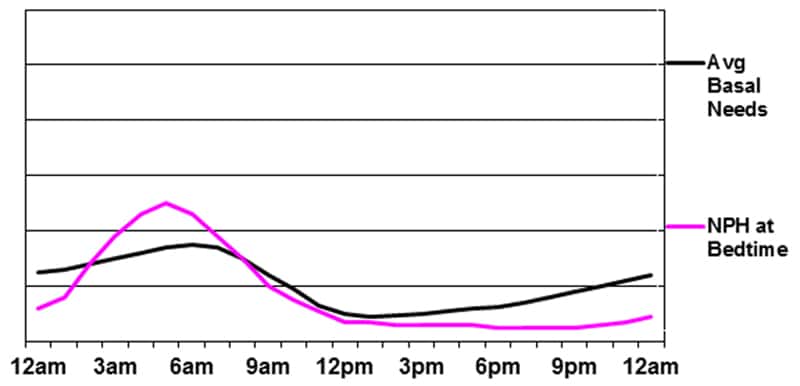
The following figures illustrate the action profiles of various types of basal insulin programs.
Basal insulin supplied by NPH at bedtime
Basal insulin supplied by NPH in the morning and evening
The advantages of this program are the peak in basal insulin during the night and the possibility of using the morning NPH peak to cover the carbs eaten at lunchtime. The drawbacks are the same as those in Figure 3 above, plus the major issue of having to conform to a rigid meal/snack schedule during the day due to the peak of the morning NPH insulin. As the graphic clearly shows, this type of basal insulin program does a poor job of matching the body’s needs. It rarely produces stable glucose levels – particularly during the daytime.
Unfortunately, those who use “premixed” insulin twice daily are, essentially, utilizing this approach for their basal program. Each injection of premixed insulin contains anywhere from 50-75% NPH insulin, with the remainder being either Regular or rapid-acting insulin.
Basal insulin supplied by glargine (Lantus) or detemir (Levemir)
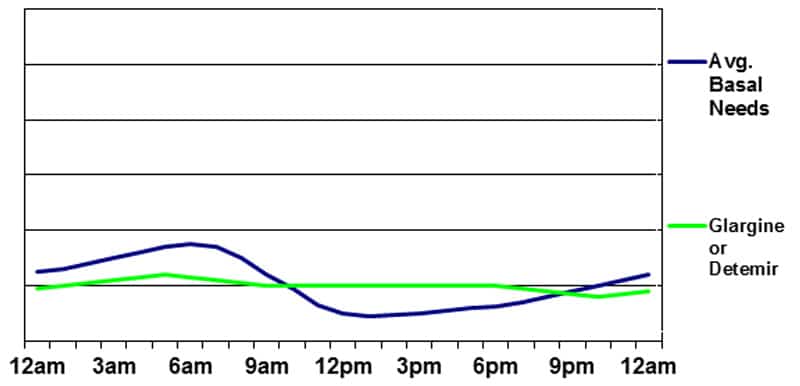
The main advantage of using glargine or detemir is the relatively unwavering flow of insulin (a very slight peak may occur 6 to 10 hours after injection of detemir) and consistent absorption pattern. The disadvantages include the potential for a gradual blood sugar rise during the night (due to the lack of a pre-dawn peak) and around the time of the injection when the insulin is taken once daily (the basal insulin may “wear off” a few hours early and take a few hours to “kick in”). There is also potential for a gradual blood sugar drop in the afternoon as the basal insulin level may exceed the liver’s production of glucose.
Basal insulin supplied by Glargine or Detemir plus Evening NPH
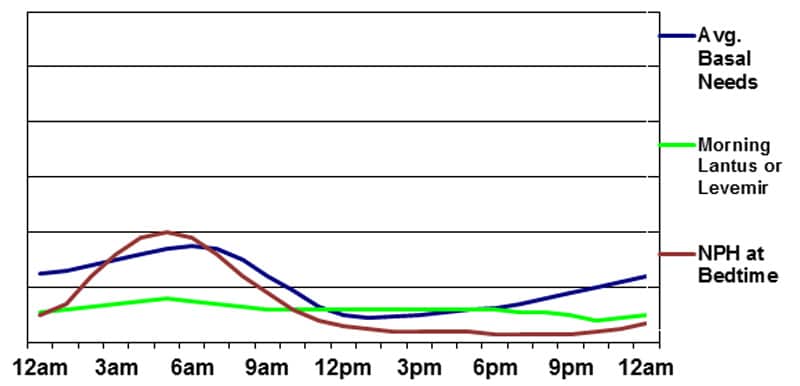
The disadvantages include the need for at least two separate injections and the filling of multiple prescriptions. There is also potential for mixing up doses or taking the wrong insulin at the wrong time since several different types of insulin are being utilized simultaneously.
Basal insulin supplied by Insulin Pump Therapy
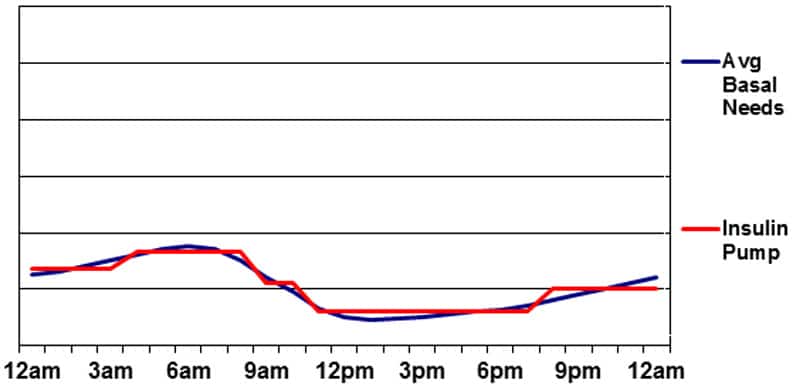
Perhaps the greatest drawback to delivering basal insulin with a pump is the risk of ketoacidosis. Any mechanical problem resulting in a lack of basal insulin delivery can result in a severe insulin deficiency in just a few hours. Without any insulin in the bloodstream, the body’s cells begin burning large amounts of fat (instead of sugar) for energy. The result is the production of acidic ketone molecules—a natural waste product of fat metabolism. This rarely occurs when taking injections of long-acting insulin since there is almost always some insulin working as long as injections are not missed.
Successful pump use will require adequate follow-up and fine-tuning. This should include:
- Basal rate testing throughout the day and night (fasting for 8- to 10-hour intervals and testing blood sugars to see if they are holding steady)
- Fine-tuning of bolus formulas (based on record-keeping)
- Troubleshooting and prevention of emergencies such as DKA (diabetic ketoacidosis); and
- Use of advanced pump features such as extended boluses and temporary basal rates.
Suggested next post: My Experiments with Managing Dawn Phenomenon
If you liked this post, please sign up for our newsletter (and get a sign-up bonus) in the form below. We send out a weekly newsletter with the latest posts and recipes from Diabetes Strong.