What is Plantar Fasciitis?
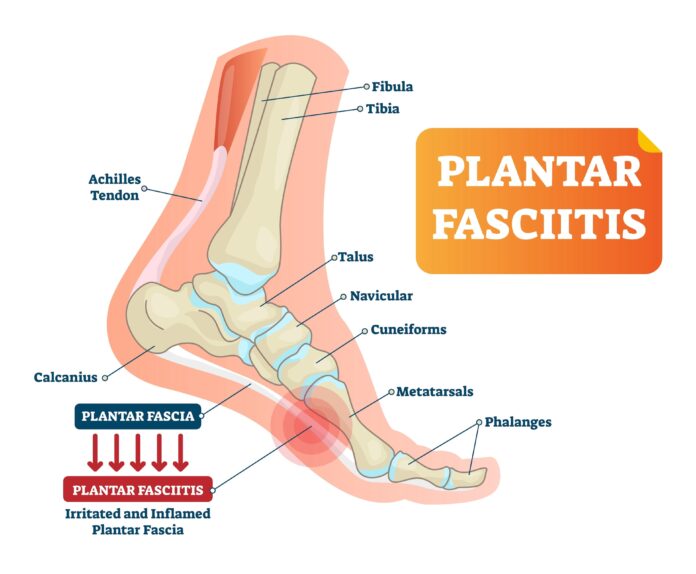
Plantar fasciitis is a prevalent and painful condition affecting the heel. It arises from inflammation of the plantar fascia, a robust, fibrous tissue band stretching along the bottom of the foot. This tissue connects the heel bone (calcaneus) to the base of the toes, playing a crucial role in supporting the foot’s arch and facilitating normal walking mechanics.
The tension in the plantar fascia increases when weight is placed on the foot, such as when standing. This tension also rises when pushing off from the ball of the foot and toes, motions essential to walking and running. Over time or excessive use, the plantar fascia can lose its elasticity and resilience, becoming irritated even during routine daily activities.
Plantar Fasciitis Causes
Plantar fasciitis results from inflammation and pain in the plantar fascia, which can be triggered by various factors, including:
- Increased Activity Levels: Starting or intensifying a walking or running program can stress the fascia.
- Foot Structure or Shape: Certain foot anatomies, such as flat feet or high arches, can predispose individuals to plantar fasciitis.
- Surface Type: Hard or uneven surfaces can exacerbate stress on the plantar fascia during standing, walking, or running.
- Inappropriate Footwear: Shoes lacking proper support or cushioning can contribute to the condition.
- Excess Weight: Additional weight places more stress on the feet, increasing the risk of plantar fasciitis.
Less commonly, plantar fasciitis can be associated with underlying medical conditions such as lupus or rheumatoid arthritis, which may contribute to plantar fascia inflammation.
What Are the Symptoms of Plantar Fasciitis?
Plantar fasciitis typically manifests as a gradual increase in pain, primarily felt near the heel. In some cases, the pain can onset suddenly, often after activities like missing a step or jumping from a height. The typical symptom is “first-step pain,” characterized by intense discomfort upon rising in the morning or after periods of inactivity.
Throughout the day, the pain may diminish as the foot warms up but can intensify again after prolonged standing, walking, or vigorous activity. Walking barefoot or wearing shoes with minimal support often exacerbates the pain.
Other symptoms may include:
- Stiffness and Limited Flexibility: Reduced range of motion in the foot due to tightness in the plantar fascia.
- Swelling: Mild swelling may be present in the heel or arch of the foot.
- Tenderness: Pressing on the heel or along the arch can provoke tenderness and discomfort.
- Burning Sensation: Some individuals report a burning or aching sensation extending from the heel along the bottom of the foot.
Understanding and recognizing these symptoms is crucial for early diagnosis and effective management of plantar fasciitis, ensuring a quicker return to pain-free activity.
What Should I Avoid with Plantar Fasciitis?
Plantar fasciitis is a serious condition that requires careful management to prevent worsening symptoms and facilitate healing. Here are key aspects to avoid and understand:
- Ignoring the Pain: Plantar fasciitis cannot be ignored. Disregarding your feet discomfort can exacerbate the condition, leading to prolonged pain and potential complications. Addressing any discomfort is crucial to prevent further aggravation.
- Wearing Improper Footwear: Opting for unsupportive footwear can worsen pain and hinder healing. Good shoes are essential not just for style but for providing the necessary support for your feet, aiding in long-term comfort and health.
- Overexerting Yourself: Engaging in high-impact activities without adequate support can strain your already sensitive feet and delay recovery. It’s important to embrace gentler activities that allow you to stay active without exacerbating your condition.
- Neglecting Stretching Exercises: It is vital to incorporate gentle stretching exercises into your routine. Neglecting these stretches can lead to a cycle of stiffness and pain. Stretching promotes flexibility and alleviates tension, helping your feet find relief.
- Delaying Medical Attention: Delaying medical attention can prolong discomfort and hinder recovery. Consulting a healthcare professional early on provides tailored solutions and effective treatment strategies, ensuring a quicker return to comfort.
Plantar Fasciitis Diagnosis
Plantar fasciitis is one of many conditions that can cause heel pain. Other potential causes include:
- Nerve Compression: In the foot or back, leading to similar pain symptoms.
- Stress Fracture of the Calcaneus: A small crack in the heel bone.
- Loss of the Fatty Tissue Pad Under the Heel: Reducing natural cushioning and increasing pain.
Distinguishing plantar fasciitis from these conditions typically involves a thorough medical history and examination by a physician.
Heel Spurs and Misconceptions
Heel spurs, often wrongly assumed to be the primary cause of heel pain, are usually the bone’s response to traction or pulling forces from the plantar fascia and other foot muscles. While common, they typically do not cause pain. A significantly enlarged and problematic heel spur requiring surgery is rare.
Understanding and addressing these aspects can significantly impact managing and recovering from plantar fasciitis, promoting foot health and overall well-being.
Plantar Fasciitis Treatment
Plantar fasciitis, a common cause of heel pain, requires prompt and appropriate management to alleviate symptoms and promote healing. Treatment duration often correlates with the severity and duration of symptoms. High-demand athletes, like marathon runners, may face longer recovery periods due to the intense strain on their feet.
Treatment Options:
- Stretching and Physical Therapy: Stretching exercises targeting the plantar fascia and Achilles tendon are highly effective. A physical therapist can guide you through exercises to perform at home, which can also strengthen lower leg muscles and stabilize the ankle.
- Icing and Medication: Applying ice to the affected area several times daily can reduce pain and inflammation. Non-steroidal anti-inflammatory drugs (NSAIDs) may also be recommended by your doctor.
- Rest, Activity Modification, and Orthotics: Reducing weight and stress on the foot is crucial for healing. Recommendations may include:
- Switching to shock-absorbing surfaces for exercise
- Wearing shoes with proper arch support or using orthotics
- Applying athletic tape to support foot muscles and ligaments
- Using night splints to maintain foot stretch during sleep
- Modifying activities, such as replacing running with swimming or cycling
- Shock Wave Therapy: This involves delivering low or high-energy shock waves to the affected area, inducing microscopic trauma that stimulates the body’s healing response.
- Steroid Injections: If symptoms persist after a few months of treatment, steroid injections may be administered to reduce inflammation.
- Gastrocnemius Recession: Surgery is rarely needed but may be considered in severe cases. This procedure involves lengthening the gastroc tendon, part of the Achilles tendon, to relieve tension on the plantar fascia.
Lifestyle Changes for Plantar Fasciitis Management
Implementing lifestyle adjustments can significantly aid in managing plantar fasciitis and preventing flare-ups.
Key Adjustments:
- Maintain a Healthy Weight: Reducing excess weight alleviates pressure on the feet, decreasing strain and facilitating a quicker recovery.
- Adopt Proper Walking and Standing Practices: Distribute weight evenly, avoid excessive heel stress, and take breaks to rest your feet.
- Use Orthotic Inserts: Orthotic inserts provide cushioning, stability, and alignment, enhancing comfort and relieving plantar fasciitis symptoms.
Daily Care Tips:
- Foot Care Routines: Regularly soak your feet in warm water, massage them, and use moisturizing creams to soothe and nurture tired soles.
- Preventive Strategies: Warm up before physical activities, wear supportive footwear, and maintain good posture to minimize strain on your feet.
- Discomfort Relief: Ice packs, foot massages, wearing compression socks and elevating your feet can reduce pain and inflammation.
Recovery Timeline
Recovery from plantar fasciitis varies. Some individuals experience relief in weeks, while others may need several months of consistent treatment. Factors influencing recovery include the condition’s severity, adherence to therapies, lifestyle modifications, and individual healing processes. Patience, diligence, and following a personalized treatment plan are essential for optimal recovery and preventing recurrences.
By understanding and implementing these treatment and lifestyle strategies, you can take proactive steps toward effectively managing plantar fasciitis, ensuring better foot health and overall well-being.
The Takeaway
Overcoming plantar fasciitis demands patience, informed choices, and dedicated self-care. Every proactive step matters in your journey to relief. Compression socks from brands like Viasox can be game-changers, boosting blood flow, reducing swelling, and providing crucial support to ease discomfort. Regular stretching, proper footwear with good arch support, and orthotic inserts are essential. Modify activities to minimize foot strain and consult healthcare professionals for a tailored treatment plan. By implementing these strategies and embracing supportive solutions, you can confidently stride towards comfort and wellness, giving your feet the care they deserve.